Guide to Sleep and PTSD
According to the National Institute of Health, Post-Traumatic Stress Disorder (PTSD) can occur in people who experience a traumatic situation and continue to have a range of "fight-or-flight" reactions long after the traumatic event. PTSD is considered a disability that greatly affects how sufferers live and work.
Statistics reveal that as many as 3.6% of U.S. adults may have PTSD and struggle with everyday tasks, including getting a good night's rest. Whether you or someone you care about has PTSD, understanding more about the condition can be the first step to living a more normal life, including during the time spent sleeping.
People with PTSD deal with the memories of their trauma in different ways, but it’s common to have more pronounced symptoms or stress from their trauma at night when they aren’t busy and can’t as easily block out recurring memories, feelings, and sensitivity to their surroundings.
What is PTSD?
PTSD, or post-traumatic stress disorder is a condition where someone who experiences something traumatic has unwanted emotional and physical reactions. It can interfere with daily functioning, as the person fails to fully process and recover from the traumatic event. PTSD shows up differently from person to person, with some experiencing symptoms many years after the event occurred.
The Relationship Between Sleep and PTSD
PTSD symptoms aren't limited to one area of a person's life. However, sleep disruptions are one of the indicators used to help make a diagnosis. Nightmares and difficulty sleeping are two factors that may signal someone is dealing with PTSD.
How Sleep Issues Affect PTSD
Living with PTSD may be challenging enough without the additional strain that poor sleep causes. The U.S. Department of Veterans Affairs (VA) says that a lack of sleep may lead to irritability and mood problems, trouble concentrating, and even thinking about suicide or acting in ways that self-harm.
One study even suggested that those who had nightmares before going into war were more likely to develop PTSD, giving a possible link even before the PTSD began.
How PTSD Affects Sleep
Sleep disturbances for those with PTSD vary from nightmares to more disruptive behavior patterns.They can happen frequently, or come on suddenly after a period of relief. Sleep issues may include one or more disorders in the same night.
Insomnia
If someone has difficulty falling asleep and staying asleep more than three nights a week, it’s considered insomnia. Those with PTSD frequently deal with insomnia, even if not diagnosed. They may be restless, fear falling asleep, and wake up too early to experience good rest.
70% of PTSD patients experience insomnia symptoms, typically due to a fear of falling asleep, having nightmares, and losing control while they sleep.
Obstructive Sleep Apnea
Obstructive sleep apnea occurs when a sleeping person’s airway collapses or narrows and obstructs airflow. It causes fragmented sleep and contributes to severe health consequences if left untreated.
Sleep apnea isn't specific to those with PTSD, but the two diagnoses commonly overlap, especially in veterans. Because sleep apnea keeps people from breathing well during their sleep, they wake up feeling unrested. It's not always apparent to the sufferer that they have sleep apnea, a diagnosis can be difficult. A sleep partner or spouse may be the first to notice the problems, but once identified through testing, solutions are available.
Using a Continuous Positive Airway Pressure (CPAP) breathing machine relieves symptoms of sleep apnea in many people and has offered some benefits to those with PTSD, too.
Nightmares and Night Terrors
Nightmares can range from reliving the trauma that occurred in a dream to experiencing frightening images about anything that disturbs sleep. As one of the most common PTSD sleep problems, it occurs in 50-70% of those with PTSD.
Night terrors are very frightening to the sufferer and can sometimes confuse those around them. Unlike nightmares, which generally happen quietly and are only noticeable to the sleeper, night terrors exhibit thrashing, yelling, or other disruptive patterns where the person experiencing them may seem awake but not be aware of what's going on.
Hyperarousal
Hyperarousal is the intense awareness of surroundings, such as sounds, lights, and pressure. The five senses become very overly perceptive. For those with PTSD, this can happen at night when trying to fall asleep, too. They are sensitive to sounds or even the room they sleep in. While in this "over-aware" state, sleeping and staying asleep becomes more difficult.
Sleep Walking
The medical term for sleepwalking is somnambulism, which simply means getting up and walking around while still asleep. While there may be no apparent risk to someone sleepwalking, it can also lead to more severe problems when a person tries to do dangerous things while asleep, such as driving or leaving the house. Those with PTSD may sleepwalk occasionally or be a regular part of their sleep disturbances.
Sleep Paralysis
One of the more confusing and scary sleep disorders someone may experience is sleep paralysis, or the temporary loss of muscle control and a feeling of being paralyzed after falling asleep or waking up from sleep.
When sleep paralysis occurs, the sleeper may often experience hallucinations, too, such as seeing an intruder in the room or feeling like they are struggling to breathe. Sleep paralysis lasts from just a few seconds to up to 20 minutes, which is more common in people with PTSD. It can happen when falling asleep or when waking up.
Addressing PTSD Sleep Issues
If you or someone you love has PTSD and sleep problems, addressing it right away is best. While it can take months or even years to completely resolve sleep issues, even small steps toward better sleep can make a big difference in how sufferers feel today. Many breakthroughs in PTSD treatment and sleep hygiene provide hope and lasting results.
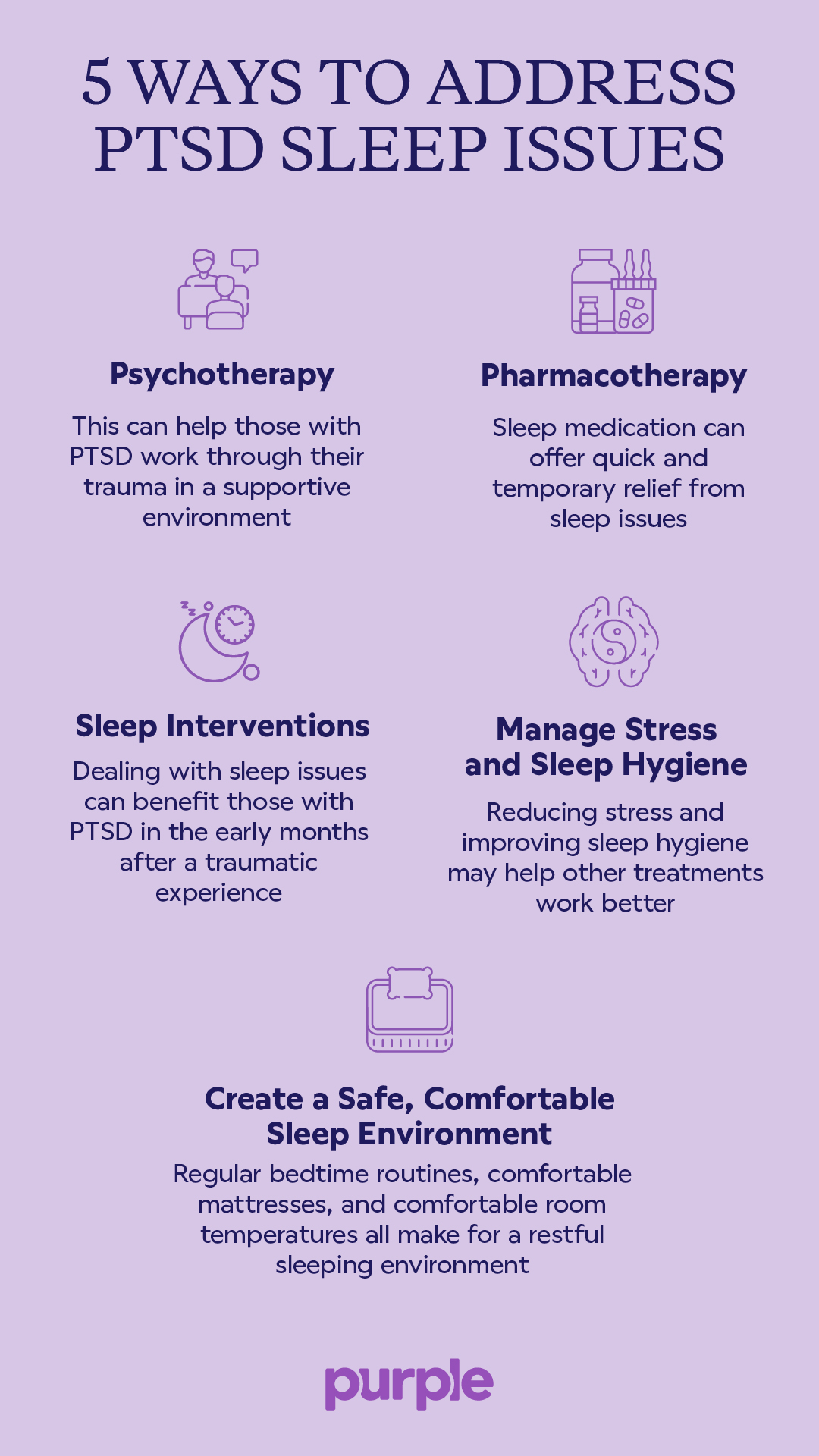
Psychotherapy
Therapy, specifically Cognitive Behavioral Therapy for Insomnia (CBT-I), can help those with PTSD work through their trauma in a supportive environment, leading to more restful sleep. The VA recommends this type of talk therapy as a more effective alternative to medication since it has improved sleep in 7 out of 10 people who tried the therapy. It can reduce nightmares and troubling sleep symptoms, as well.
CBT-I works by helping the patient learn about their sleep attitudes and beliefs, then look at the behaviors that affect their sleep. Through consecutive talk therapy sessions, journaling, and tracking sleep, patients uncover the techniques that can work for them in the long term.
Pharmacotherapy:
The VA sometimes recommends sleep medication to get quick and temporary relief from sleep issues. These can be natural supplements, over-the-counter remedies, or prescription drugs taken under the supervision of a doctor. Each medication has risks and side effects, so ask questions before taking anything you need clarification on, and don't expect it to be a lifelong remedy or a replacement for the more long-term therapy options. Most sleep aids are designed to be taken for no more than two to four weeks at a time. Some medications, such as Xanax, Valium, Ativan, and Klonopin, fall into the Benzodiazepine family; the VA doesn’t recommend these for PTSD treatment.
Sleep Interventions in the Early Aftermath of Trauma
Those dealing with PTSD may not know which symptoms to target first, but studies support the idea that dealing with sleep issues can benefit these patients as a whole. In fact, among both military and non-military groups, psychotherapy treatments that targeted sleep directly had better outcomes than those that didn't.
So, while it may not initially seem that sleep issues are the most important things to deal with, the data shows they can be more effectively influenced, especially in the early months after a traumatic experience.
Manage Stress and Sleep Hygiene
Sleep hygiene is the maintenance of a healthy sleep environment and the habits that promote sleep. While not always enough on its own, reducing stress and improving sleep hygiene may help other treatments work better.
You can work to be less anxious before bed by limiting your intake of caffeinated drinks or keeping smartphones out of the bedroom. Avoid scary or exciting movies before bed, and be sure you get to bed at the same time every night. Improving sleep hygiene is likely a part of any cognitive behavior therapy program.
Create a Safe, Comfortable Sleep Environment
Managing PTSD may take a long time. There will be good nights and bad, even after help is found. To ensure the best sleep possible, set up a regular bedtime routine in a sleep environment that supports rest.
Start with a quality, comfortable mattress that reduces vibrations from movement during the night. Since those with PTSD may toss, turn, and move a lot, this can help both partners get their best shut-eye.
Keep the room at a comfortable temperature, block out any distracting light or noise, and consider a white noise machine or fan to prevent unnecessary stimulation.
Sleep Tips for Partners of People with PTSD
It can be tough on the partners of those with PTSD to watch them struggle with the effects of trauma on their sleep. It can also affect how much sleep they get. From being woken up many times during the night from nightmares or night terrors to feeling guilty about being the only one sleeping, the relationship can feel strained over the situation.
Creating and maintaining a restful sleep environment and supporting attempts at good sleep hygiene is vital. Partners can prioritize good sleep and help set up their loved ones for success by respecting bedtime routines and doing their best to not schedule loud or busy activities during the time they normally rest. Being understanding of their partner's needs can go a long way in helping them.
If a partner with PTSD acts out in their sleep, violently or loudly, sleeping in a separate, safe area may be best. Be sure to tell your partner what's happening while they sleep so they have all the information to speak to their health professional.
Additional Resources on Sleep and PTSD
The Foundation for Post-Traumatic Healing and Complex Trauma Research
Neuroscientists learn why PTSD patients relive highly charged fear memories in sleep
National Institute of Mental Health
Sleep and PTSD FAQ
How common are sleep problems for those with PTSD?
Almost everyone with PTSD will have sleep problems, including nightmares and insomnia. These two sleep disorders are symptoms that, when observed, help doctors diagnose PTSD.
Will alcohol, marijuana, or other drugs help someone with PTSD fall asleep?
According to the VA, using these substances increases the risk of suicidal thoughts and suicide attempts. Other, more effective treatments, such as approved sleep medications and talk therapy, are safer.
Do sleep problems go away for someone with PTSD?
Therapy and changes in sleep hygiene can have a positive effect on those with PTSD, but sleep problems may not go away entirely. Every improvement in sleep can make a difference, however, so getting help and creating a plan for addressing sleep problems should be a high priority for PTSD sufferers and their loved ones.
What are some of the sleep problems someone with PTSD may have?
Sleep issues vary by person but can include insomnia, nightmares, night terrors, sleep apnea, sleep paralysis, and general difficulty getting restful sleep. Someone may experience one or all of these problems, or have different sleep issues over time.